How should Europe deal with the COVID-19 pandemic in the future?
24 August 2021
A European perspective.
In spring, many European countries relaxed or even completely lifted their containment measures following a significant drop in the incidence of COVID-19. Yet, the number of infections has increased as a result of the spread of the new delta variant.
While vaccination turns out to be very effective in protecting against a severe course of infection, people who have already been vaccinated can still transmit the virus.
How should Europe act, what strategies should it adopt, and what specific risks should it consider moving forward?
Prof. Rudi Balling, director of the Luxembourg Centre for Systems Biomedicine (LCSB), and Assistant Prof. Enrico Glab, head of the Biomedical Data Science group at the LCSB contributed to a detailed situation analysis for the coming months and years along. The initiative stems from researchers from the Max Planck Institute for Dynamics and Self-Organisation which brought together more than two dozen experts from all over Europe.
Together, they derived various possible scenarios for the future and explained what conditions would have to precede each of them
Scenario 01
Countries continue to rapidly lift restrictions
In the first case scenario, countries continue to rapidly lift restrictions, assuming the combination of past natural exposure and current vaccination coverage would allow a high incidence to continue, without overburdening health-care systems.
Given immunisation levels as of August 2021, this strategy can lead to an incidence of several hundred cases per million per day.
Scenario 02
Countries only lift restrictions at the pace of vaccination progress
In the second case scenario, countries lift restrictions at the pace of vaccination progress with the core aim to keep incidence low, given this effectively and efficiently controls the pandemic via test-trace-isolate (TTI) programmes.
This strategy would require an incidence of well below one hundred cases per million per day.
We are all in this together
In the absence of a common strategy, such a discrepancy could cause considerable friction between EU Member States, hampering cooperation, the economy and international trade: a high incidence in one country jeopardises the low incidence strategy in a neighbouring country.
“Either strategy can only work effectively if Europe agrees on a common approach. We know very well that no country will be able to stop the pandemic on its own, so it is high time for a coordinated response.”
Enrico Glaab, Head of the Biomedical Data Science group at the LCSB
Why scenario 2 of keeping incidence low is an act of solidarity
Favouring a low incidence strategy brings many advantages:
- Fewer mortality, morbidity, and long COVID
- Solidarity with those not yet protected
- Lower risk of new variants of concern emerging and spreading
- Increased feasibility of comprehensive test-trace-isolate progammes
- Fewer workforce in quarantine and isolation
- Ensuring schools and childcare remain open in the coming autumn-winter season
In light of the clear benefits of keeping incidence low, the lack of vaccination coverage in many European countries, the uncertainties about vaccinating children, and the time needed to fully vaccinate adolescents, all European countries will need to work together to achieve low incidence.
“A high incidence in one country challenges the pandemic response for others, in Europe and across the world.”
Rudi Balling, director of the Luxembourg Centre for Systems Biomedicine (LCSB), and the two dozen experts who collaborated for this article
Maintaining a low incidence is an act of solidarity and becomes easier with the benefit of increasing vaccination coverage.
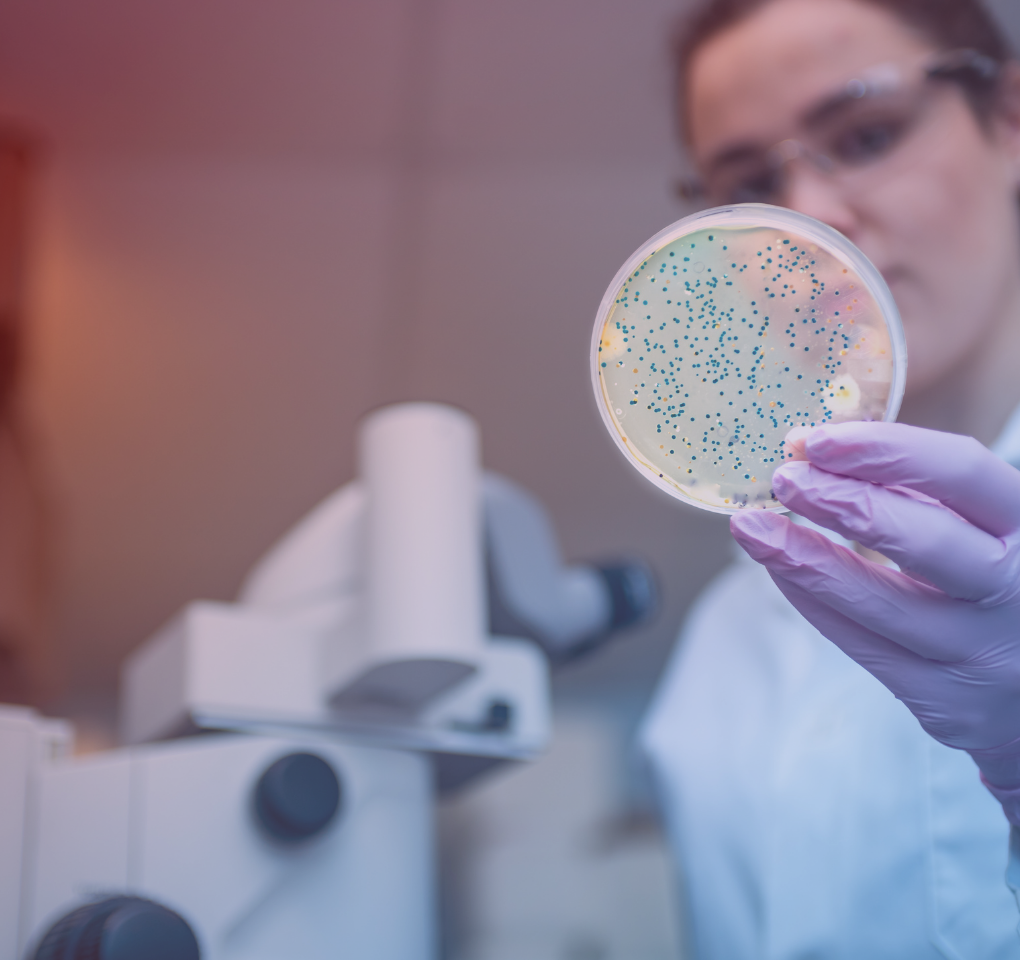
Challenges to improve measure effectiveness
Three other challenges need to be addressed to improve the effectiveness of measures.
Three challenges
01
Availability, access and reluctance to vaccinate.
02
The widespread misconception that freedom would be maximised by ignoring high incidence, whereas it has been recognised that low incidence facilitates containment and preserves freedom for all, including the most vulnerable.
03
The lack of a coherent pandemic response and communication strategy. .Risk perception, motivation and health literacy are important predictors of health-seeking behaviour and adherence to measures. Public confidence is a priority. As such, it is critical to maintain it through timely, consistent and persistent communications. This includes systematically developing a counter-speech in the event of misinformation.
The pandemic is not yet over, but an end is within reach. Restrictions can be lifted when high vaccination coverage is achieved, and if vaccines remain highly effective against VOCs.
Maintaining and communicating a clear strategy is essential, and pan-European coordination and common goals between countries are becoming increasingly critical.
Read the publication “Towards a European strategy to address the COVID-19 pandemic”, published The Lancet and The Lancet Regional Health – Europe.