Diabetes: Paving the way for a distinction between depression, distress, and burnout
31 August 2021
Precision medicine in diabetes.
People with type 1 diabetes can experience psychological health issues related to their disease. Diabetes distress, diabetes burnout & depression are frequently reported.
Yet, it is still complex, for both patients and healthcare professionals, to put the right name on their psychological complications.
How are depression in diabetes, diabetes distress, and diabetes burnout characterised? Why is it critical to distinguish one from the other?
A new study, led by Dr Gloria Aguayo with the contribution of Dr Guy Fagherazzi from the Luxembourg Institute of Health in cooperation with researchers from the CUNY School of Medicine in New York, is addressing the concepts of distress, exhaustion and depression in type 1 diabetes.
The first and most comprehensive scoping review
Psychosocial issues are among the most common complications associated with and affecting type 1 diabetes. Depression and diabetes-related distress are frequently described and associated with poorer metabolic outcomes. Diabetes burnout has recently emerged. Yet, it is unclear whether these concepts are entirely distinct or whether they overlap.
“Unraveling the concepts of distress, burnout, and depression in type 1 diabetes: A scoping review” is the first and most comprehensive study summarising how the three concepts are used in papers examining depression, diabetes-related distress and diabetes-related burnout in people living with type 1 diabetes.
Areas of overlap among the three concepts
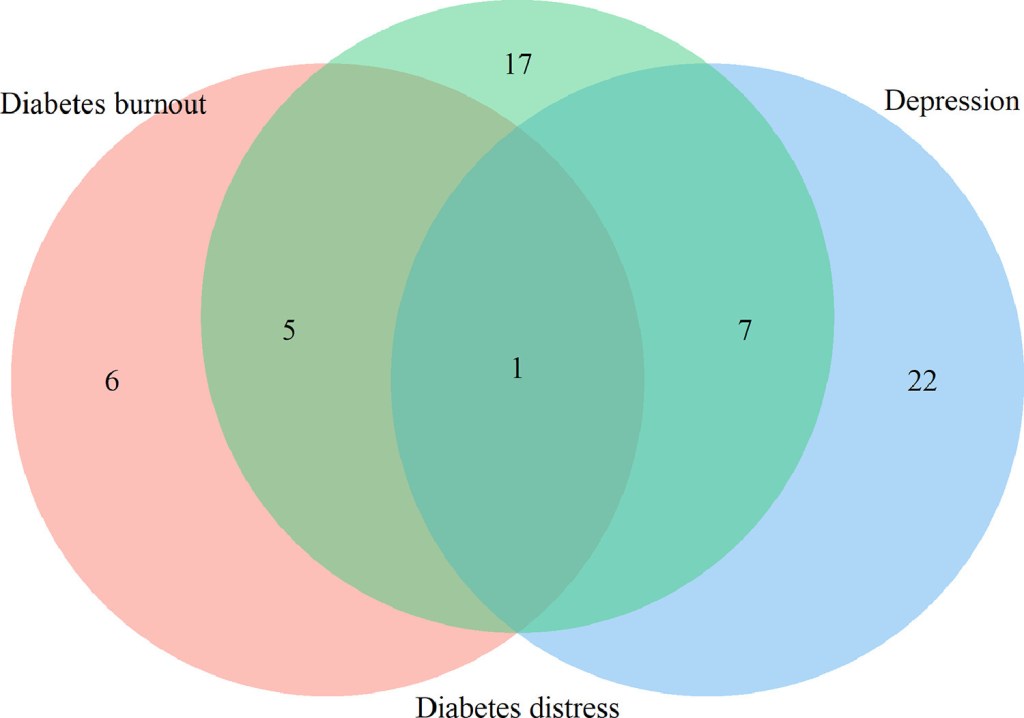
One sentence is common for the three concepts “Detachment from support systems”.
Overlapping between depression (blue) and diabetes distress (green) is in seven more sub concepts: “Fear”, “Feeling guilty”, “Feeling of failure”, “Lonely”, “Loss of energy”, “Negative mood” and “Poor concentration”.
Overlapping between diabetes distress (green) and diabetes burnout (salmon) is in five more sentences/words: “Anger”, “Burned-out”, “Frustration”, “Overwhelmed” and “Powerlessness to manage diabetes”. Twenty-two (73%), 17 (57%) and five sentences (45%) do not overlap in depression, diabetes distress and diabetes burnout, respectively.
Clarifying the underlying concepts of three psychological problems
Depression is a widespread psychological comorbidity in type 1 diabetes, although it is not specific. This condition is assessed using a variety of questionnaires, which increases the heterogeneity of the concept and increases the likelihood of overlap.
Diabetes distress is also common yet specific, and despite some overlap with depression, it seems to be an independent and different concept.
As diabetes burnout is emerging as a concept in type 1 diabetes, while being commonly mentioned in studies of diabetes distress, and presenting overlapping sub-concepts, there is a need to better conceptualise it to differentiate it from diabetes distress.
Towards better recognition and treatment
When depressive symptoms are detected using a self-reported instrument, clinicians should be aware that because of the possible overlap with diabetes distress, this diagnosis should also be evaluated.
The same situation may occur when diabetes-related distress is detected, in which case a diagnosis of diabetes-related burnout should also be screened.
Early differentiation of these concepts will allow for better recognition and treatment of the psycho-social problem with the right approach.

“Next steps are to perform data-driven analyses of qualitative studies and expert opinion with the objective of further refine these concepts. Another step should be to further analyse diabetes burnout and its differentiation from diabetes distress in clinical studies.”
Dr Gloria Aguayo, Deep Digital Phenotyping Research Unit, Department of Population Health, Luxembourg Institute of Health
Read open access study “Unraveling the concepts of distress, burnout, and depression in type 1 diabetes: A scoping review“, published by The Lancet.