Cutting-edge research in Luxembourg: A Drug Slows Down Leukaemia Progression by Blocking Cancer-Causing Genes
18 July 2023
Revolutionary Breakthrough for Slowing Down Leukaemia
Luxembourg scientists demonstrate the therapeutic value of a compound that inhibits oncogene translation.
Researchers from the Luxembourg Institute of Health reveal the ground-breaking therapeutic potential of the compound FL3 in inhibiting oncogene translation and rewiring cancer cell metabolism, opening up new therapeutic opportunities for leukaemia patients.
In a remarkable new development, scientists at the Department of Cancer Research (DoCR) at the Luxembourg Institute of Health (LIH) have demonstrated the powerful impact of a drug in slowing down the progression of leukaemia by blocking the activation of cancer-causing genes. The findings, recently published in the prestigious international journal Blood (open-access), offer new hope for patients with chronic lymphocytic leukaemia (CLL) and pave the way for innovative therapeutic avenues against cancer.
Impending cancer cell growth
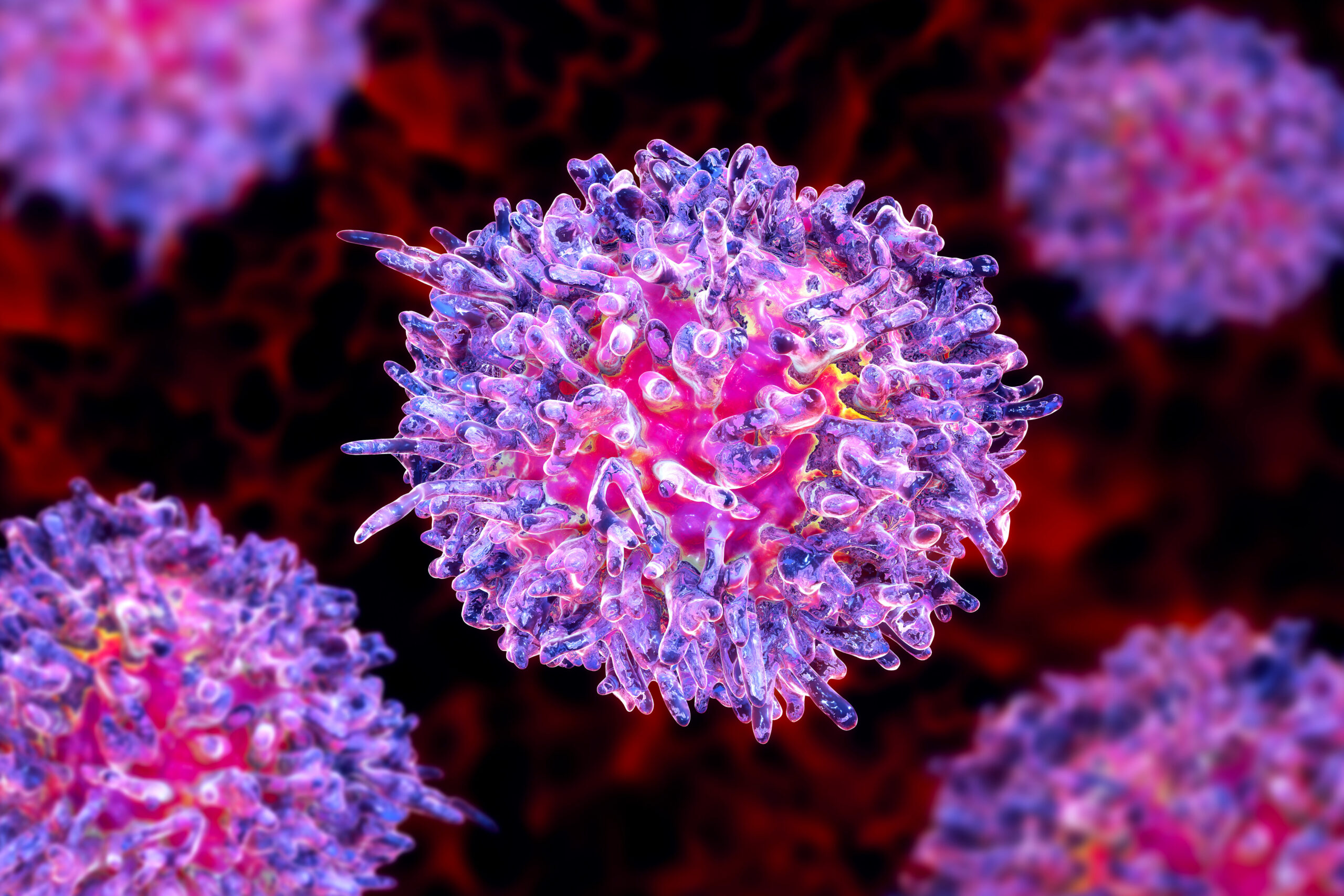
Leukaemia, particularly CLL, is a prevalent form of cancer characterized by the overproduction and accumulation of dysfunctional B lymphocytes in various parts of the body. This study focused on inhibiting the translation (i.e. the cellular process producing proteins) of oncogenes, specifically the MYC gene, within CLL cells to rewire their metabolism and reduce their ability to multiply rapidly, thus impeding the advancement of the disease.
Led by Drs Jérôme Paggetti and Etienne Moussay, the pioneering researchers from the LIH Tumour Stroma Interactions (TSI) research group conducted extensive investigations using patient samples and animal models. The team demonstrated that synthetic flavagline FL3, a known inducer of cancer cell death, effectively inhibits translation and synthesis of proteins associated with key cellular processes.
The study also revealed that CLL cells derived from patients exhibited greater sensitivity to FL3-induced death compared to healthy cells. Furthermore, by inhibiting MYC translation, low doses of FL3 induced significant changes in cellular metabolism, blocking the cell cycle and impairing growth and proliferation of both human and animal CLL cells. These findings provide strong evidence supporting the use of translation inhibitors as a selective therapeutic approach for treating CLL.
Excitingly, the researchers identified that FL3 specifically targets a group of proteins called prohibitins (PHBs) that they proved to be directly involved in translation. By disrupting the interaction between PHBs and the translation machinery, the drug FL3 hinders the initiation of translation, effectively interfering with the process and impeding cancer cell growth.
To validate the efficacy of FL3 in slowing down CLL progression, the researchers conducted in vivo experiments on mice. The results were astounding, as the treatment drastically reduced the percentage of CLL cells in the spleen and significantly improved overall survival rates. Importantly, FL3 selectively targeted malignant CLL cells without affecting healthy B cells, thus providing a promising strategy for selectively combating cancerous cells while leaving healthy cells unharmed.
Intriguingly, when FL3 was combined with anti-PD1 immunotherapy, the outcomes were even more impressive, indicating that FL3 may also enhance anti-tumour immunity.
New therapeutic opportunities
Our research unveils a highly translational dimension to the field of CLL treatment. We found that high expression of translation initiation-related genes and PHBs genes correlates with disease progression, poor survival, and unfavourable clinical parameters in CLL patients. By inhibiting translation, we can potentially overcome treatment resistance and offer a promising approach to tackling relapse in this challenging malignancy.
Dr Anne Largeot, senior scientist within the TSI group and the first author of the study
The study, titled “Inhibition of MYC Translation through Targeting of the Newly Identified PHB-eIF4F Complex as Therapeutic Strategy in CLL,” was not only published in the prestigious journal Blood but also featured on its cover page, highlighting the significance of this research.
This study was made possible through generous support from the Luxembourg National Research Fund (FNR), Fondation Cancer, FNRS-Télévie, Plooschter Projet, the Belgian Foundation for Cancer Research, the Swedish Children’s Cancer Foundation, the Swedish Research Council, and the Swedish Cancer Society.