COVID-19: Why is it possible to protect yourself and others by using vaccines and what are the underlying principles?
23 March 2021
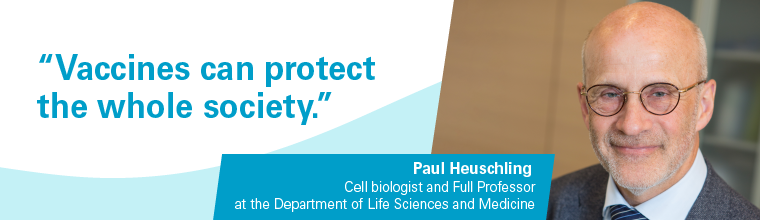
Pathogens such as viruses have always existed together with mankind. In this interview, Paul Heuschling, cell biologist and full Professor at the Department of Life Sciences and Medicine, explains the process of vaccine development. He elucidates how they can protect us due to immunisation and what are the underlying principles of the new mRNA vaccination technology.
This article was originally published by the University of Luxembourg
By now, several COVID-19 vaccines have been released. How can we be sure that they are working?
The strategies that are used to design any vaccine aim to achieve the highest possible immune outcome. That means, already at a very early stage in development researchers check the immune response of the body and will reject the vaccine if it is not good enough. So, the fact that a vaccine reliably generates an immune response is one of the prerequisites during vaccine development. Since viral protein structures as well as weakened or dead viral particles are typically used for this, the mounted immune response can be expected to be very similar to the one generated by the pathogen itself.
In quantitative terms, the functionality of the vaccine is expressed by its efficacy which is determined in clinical studies. The commonly reported efficacies of more than 90% for most of the COVID-19 vaccines show that they indeed succeed in mounting a specific immune response against SARS-CoV-2.
How is such an immune response generated in the body?
When an immune reaction is generated by the body, it recognises something that the virus exposes – in most cases these are proteins. Proteins are among the most important building blocks of life and can acquire many different shapes and functions. Ultimately, we are also to a large extend made out of various proteins. However, every organism and also viruses have a specific set of proteins with typical patterns and structures that differentiate them. This is why our immune system is able to recognise a viral protein structure, which is also called antigen in this context, as foreign: That protein does not have a shape or constitution that is known or typical for the own body.
Is this also the principle used in vaccine development?
Generally speaking, yes. The traditional way to create a vaccine is to cultivate the virus in the laboratory, harvest it and inactivate its function to infect cells, for example by chemical treatment. What remains are virus particles including viral proteins, that are not harmful to the body anymore, but still can trigger an immune reaction upon injection. This can prime the immune system to the specific pathogen and will induce the production of specific antibodies neutralising the antigens as well as other immune cell reactions. If then in the future a contact with the real virus occurs, the immune system is prepared already and can immediately initiate the production of specific antibodies necessary to fight the virus.
A drawback in this approach of vaccine development is the rather time-consuming process in production and the low throughput. Culturing the virus in the laboratory is not easy and requires some time for the virus to grow and also to treat it afterwards for inactivation. That means producing high amounts of vaccine using this method is challenging and both expensive and time-consuming.
Which other approaches exist to develop a vaccine?
Instead of injecting inactivated viral particles, it is also possible to produce parts of a viral protein directly inside the human cell by introducing the blueprint for that particular antigen. This approach is commonly used in vaccinations against tuberculosis, for example. A part of the genetic information of the pathogen is introduced into a carrier-vessel, typically an adenovirus. That virus which normally causes a form of common cold in some primates, is also modified so that it cannot cause disease anymore. As a result, only in a defined area cells of our body are infected: The vessel delivers the genetic material of the virus in these cells and they then produce desired antigen, which triggers the immune system. The advantage is that the adenovirus containing the blueprint for the antigen can easily be produced in the lab while at the same time it cannot cause an infection. The vaccines against SARS-CoV-2 developed by AstraZeneca and the Russian Gam-COVID-Vac, also known as Sputnik V, use this approach.
However, since several years a new technology was developed which bypasses the use of an adenovirus as a carrier vessel: Instead of introducing the blueprint into this adenovirus, it is contained in small lipid droplets as mRNA, a short-lived genetic blueprint which is chemically different from our genomic DNA. Like in the case of the adenovector-based vaccines, this genetic material can enter the cell and serve as a blueprint to produce the viral antigen. This new technology is used in the two vaccines by Pfizer/BioNTech and Moderna and allows the production of comparably large amounts of vaccine. It should be stressed that the mRNA technology has been developed already since around a decade and SARS-CoV-2 only by incident happens to be the target of the first approved mRNA vaccine. It is very likely that other mRNA-based medications will soon be available as well and might bring great progress to medicine.
Isn’t it dangerous to inject genetic material into a cell?
First of all, we should remember that this is exactly what happens upon a viral infection, including the common cold: The virus introduces its genetic material into our cells and uses the machinery of the cell to generate complete and therefore infectious copies of itself. So, the new mRNA technology as well as the long-known adenovirus-based vaccines make use of the same principle while only inducing the production of a non-infectious antigen inside the cell. The most important difference is that only a small and harmless piece of the virus, one particular part of a protein, is produced. Therefore, no infection can occur or affect other cells.
Second, the injected mRNA contains a genetic signal that a protein should be produced from it, also indicated by the ‘m’ which stands for messenger. RNA is fundamentally different from DNA which resides in the nucleus of our cells and does not get close to this mRNA. At the same time, also our own cells all the time make hundreds of different mRNAs to produce the proteins which ensure the vital functions of our cells. In other words, as our own cells anyways constantly produce proteins from many different mRNAs, there is no reason to assume any danger from this technology.
Finally, RNA generally is quite fragile. This is also one of the reasons why some of these vaccines need to be stored at very cold temperatures as low as -80°C to ensure the efficacy of the vaccine. After the injection, the RNA is typically degraded within hours and thus does not have any long-term impact, while this time is still sufficient to produce the antigen and trigger the immune system’s response.
How can it be that a vaccine against a previously unknown virus was developed so fast?
First of all, it is important to know that the SARS-CoV-2 is not the first coronavirus we encounter. We have learned a lot from the previous appearance of the SARS-1 and the MERS coronavirus, not to forget the several other types of coronaviruses causing mild infections each year, such as the common cold. Therefore, we knew the basic building blocks of this type of virus and the best leverage points for a vaccine. Also, several scientific groups worldwide focused on research on coronaviruses during the past years and readily shared their knowledge with others.
In addition to that, often a limiting factor for scientific development is the availability of resources and money. As governments and stakeholders quickly realised the threat caused by this virus, all efforts have been merged to provide any financial support required. And as unfortunately many people were rapidly infected with the virus, in turn also volunteers for clinical studies could easily be identified. At the same time, all tests and protocols to assess and determine the safety of the vaccine were kept in place. A fast and efficient exchange with the health and drug authorities additionally helped to accelerate the process. That means no tests were skipped and the COVID-19 vaccines can be expected to be as safe as any other vaccine on the market.
What would happen if we had no vaccine available?
Well, this somehow would resemble the natural process: If a virus runs free within a population, some individual will eventually become immune after an infection whereas the disease will have more severe consequences or can even be lethal for others. This would continue until a certain percentage of the population is immune, which is estimated to be around 70%. At such a turning point, the virus statistically could not be transmitted to enough susceptible individuals and thus the infection would decay.
However, until we reach such a level of herd immunity, we would lose a significant part of our population, especially in the older generation.
With the vaccination being available we do now have the chance to actively increase the overall immunity in society to arrive faster at this turning point – without having to be infected by the real virus. And in quantitative terms, the absolute number of complications such as allergic reaction simply does not compare to the damage the virus does. It is difficult to give exact numbers, but the overall damage caused by the virus without vaccination is several orders of magnitude higher than any potential harm caused by a vaccination.
I therefore can only encourage everyone to get the jab and participate in that societal effort to bring the virus under contro
Paul Heuschling is Full Professor in Cell Biology at the Department of Life Sciences and Medicine at the University of Luxembourg. His research is focused on inflammation of the central nervous system and on glia cells.
This article was originally published by the University of Luxembourg